River's Road Home
Respiratory Therapy and Parent Training Pave the Path from Hospital to Home.
Ana Rivera found out she was pregnant on Halloween in 2020. She and her partner, Diana Vasquez, started preparing for the next chapter in their lives and their new arrival.
However, on April 8, 2021, at just 26 weeks’ gestation, River Omari Rivera was born weighing a mere 2 lbs., 2 oz. and was just 14 inches long. Due to his extreme prematurity, Ana and Diana found that he barely fit in their hands, comparing him to the size of a water bottle. They were afraid to touch him for fear of hurting him.

While Rivera was recovering from pre-eclampsia, she remembers getting a call from the NICU downstairs in the hospital.
"Someone called me and said, 'His lungs are not taking'," remembers Rivera. "And that's when he went on the first breathing apparatus."
As a micro preemie, River was diagnosed with severe bronchopulmonary dysplasia, requiring mechanical ventilation in order to breathe.
"The way it was explained to us was that his lungs were a muscle, and he could not open and close them on his own," said Vasquez. "Normally, in kids with his condition, they don't last too long, and they were trying to give us the reality of our circumstance."
Rivera and Vasquez were determined to help River grow and took things day by day. To capture his milestones, they took photos on the 8th day of every month.
"Every month that he grew another thirty days, we decided to have a photoshoot," said Vasquez. "His first costume, he was a nurse. From there, he was also a cop, a fireman, and baby Yoda."
After seven months in the NICU, River was admitted to Blythedale Children's Hospital for comprehensive pulmonary rehabilitation and post acute neonatal care.
The NICU nurses instilled in us that life was going to start once we got to Blythedale," said Vasquez.

Rivera and Vasquez immediately noticed a difference when they entered Blythedale Children's Hospital. "You immediately saw that there was going to be a nurse there for him. But in our minds, it was we need to care for him, we need to play with him and we to hold him. We felt like moms," said Rivera.
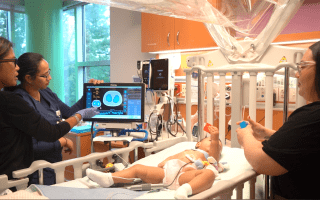
At Blythedale Children’s Hospital, where more than a third of the patients are admitted for intensive pulmonary rehabilitation, there is a dedicated clinical care team following countless protocols and measures in place to ensure that children, like River, ranging from tiny prematurely born infants through adolescents, can breathe with ease and, often, take their first breath free from mechanical ventilation. One of River's Respiratory Therapists, was Christine Stack, RRT. As his therapist, Stack would measure his End Tidal Carbon Dioxide levels (ETCO2) to assess how well he was ventilating, as well as his positive end-expiratory pressure (PEEP). River's PEEP pressure evaluated the amount of positive pressure that remained in the airways at the end of his breathing cycle.

"When he got here, his end tidals were in the 100s. Your end tidals should be 35-45," Stack said, emphasizing his fragile state. "And his PEEP pressures, his pressure support, they were huge. They were 14, the average is 5."
Stack, along with River's medical team and rehabilitation therapists, helped him continue to grow. Each day, River would receive comprehensive therapies, including physical, occupational, speech and feeding, as well as developmental support to help him reach important milestones.
"It made me feel comfortable to watch the therapists and teachers work with River. To watch them, it took the fear of the tubing away," said Vasquez. "We realized he can do everything a regular child does, he just has an extra attachment."
Dean Soto, MPA, RRT, AE-C, Assistant Director of Respiratory Therapy also helped take the fear of the tubing away for Rivera and Vasquez through Blythedale's comprehensive Parent and Family Education Program.

"One thing I've noticed is that if someone is afraid of something, they won't touch it," said Soto. "It's difficult at first but once parents realize that a ventilator is just an extension of the child and they learn how to overcome some of the challenges and the fears of the alarms, it becomes, 'Oh, I can do this,' and that is so rewarding to see."
Rivera and Vasquez began to train with Soto, learning how to care for River and understand his ventilator settings. Through Blythedale's new state-of-the-art Simulation Lab, comprised of high-tech spaces that replicate bedside and home environments, parents can learn how to care for their medically fragile child in a supportive, controlled environment, in preparation of their discharge home. They also trained with Angela Larkin, RN, MSN, Child and Family Education Coordinator and Corinne Oppedisano, RN, Child and Family Educator to learn how to change River's gastronomy tube, his tracheostomy tube, and how to set-up their own home once they discharged.

"I really liked working with Angela," said Rivera. "I felt like she really listened to us and she gave us good confidence. And Corinne, she took the time to train my mom who wanted to train so that she could help her grandson."
River's path home wasn't always linear though. As River started using his own respiratory muscles and expending so much energy to breathe, he began losing weight.
"When River began losing weight, the team increased his calorie count and worked on a different plan to work through his disease process," said Soto. "As those started to improve and his respiratory muscles got stronger, he began breathing on his own and we were able to begin weaning him off of the ventilator."
On September 8, 2022, River was discharged home, breathing on his own, requiring supplemental oxygen only at night.
"It's still a journey and road that we have to get to," said Rivera. "But we're home and we can be a family as one."

While in the NICU, Rivera and Vasquez would often go to Wood & Fire in Pleasantville, NY during shift changes. At the restaurant, they'd daydream about bringing River to the restaurant so they could be one as a family. Two days after he was discharged, Rivera had an idea. "I put a onesie on him that said, 'Will you take our last name?'" said Rivera. Without Vasquez knowing, Rivera covered up the onesie with another shirt.
"At the restaurant, while Diana was in the bathroom, I changed his shirt to the onesie," said Rivera. "When she came back, I told her he had spit up. Diana's initial instinct was, 'Let me see him!' So I told her to look at his shirt. That's when she saw it and saw me there popping this question."

In the background was the waitress, filming the moment. Though the waitress at first didn't know it, she said to them, "Wow you're finally here as a family at this table."
It's still a journey and road that we have to get through," said Rivera. "But we're home and we can be a family as one."